The MAP model: approaching behaviour change conversations on farm
Laura Gribben BSc MSci, PhD student at Queen’s University Belfast and Teagasc Walsh Scholar, and Alison Burrell MSc, CPsychol Ps SI, Chartered Health Psychologist at Animal Health Ireland (AHI)) outline the MAP Model of behaviour change and its use as a tool to structure behaviour change conversations on farm
With the increasing focus on preventative medicine, herd health management and sustainability, farmers are continually being challenged to make changes to their farm routine and farm behaviours (Bord Bia, 2022; Svensson et al., 2022). In this context, the role of the veterinary practitioner becomes ever more critical as an advocate for change. However, to fulfil the potential of this role, it has been recognised that veterinary practitioners could benefit from training in evidence-based communication strategies, specifically designed to support behaviour change (Bard et al. 2019). The behavioural sciences such as health psychology have extensively studied the area of behaviour change, exploring its theoretical underpinnings and developing strategies which can be used to encourage it. This has led to a growing interest in adapting behavioural science-based behaviour change communication strategies to the field of veterinary medicine (Svensson et al. 2020a; 2020b; Bard 2018). One such behaviour change communication strategy which may be applicable is the MAP (Motivation, Action and Prompts) of Behaviour Change model (NHS Education for Scotland (NES), 2022).
What is the MAP model?
MAP was originally designed to provide health and social care professionals with a communication framework for having behaviour change conversations with patients (NES, 2022). It was designed to be equally useful for short, opportunistic health consults (such as a pharmacist delivering a smoking cessation consult to a customer) or longer, more structured consults (such as a nurse practitioner working with patients on a cardiology rehabilitation programme) (NES, 2022). Delivering the MAP model involves using person-centred communication skills and working through three steps with clients. In steps one and two, professionals gather information on their client’s individual circumstances and identify where their client is in the process of changing (NES, 2022). In step three, professionals provide tailored support based on the client’s stage of change, by utilising behaviour change techniques (BCTs) (NES, 2022).
BCTs are defined as the ‘active ingredients’ or detectable, replicable elements of behavioural interventions designed to change behaviour (Michie et al., 2013). An example of a BCT is using a pedometer or smart watch for self-monitoring physical activity. Over 90 different BCTs have been identified by behavioural scientists (Michie et al., 2013). Commonly used BCTs include: action planning, goal setting, and exploring the pros and cons of a behaviour. Several reviews in the area of health behaviour change have identified that the use of BCTs has had a positive outcome on behaviour and health. Avery et al. (2012) identified that use of the goal setting, problem solving and social support BCTs in studies designed to promote physical activity in diabetes patients, was linked with a beneficial reduction in HbA(1C), a measure of blood glucose regulation. While Ashton et al. (2020) found that the use of the social support and self-monitoring of behaviour BCTs were associated with improved outcomes in weight management interventions in young adults. Patterson et al. (2022) found that the use of the action planning BCT was associated with an increase in physical activity in patients with cardiovascular disease.
How was the MAP model developed?
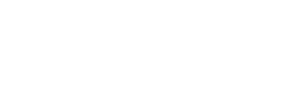
The MAP model was introduced in the NHS Health Behaviour Change Competency (HBCC) Framework and was subsequently developed into a training programme by health psychologists based in NHS Education for Scotland (NES) (NES, 2022; Dixon and Johnston, 2010). The HBCC Framework created the MAP model by integrating several different behavioural theories (Dixon and Johnston, 2010). It specified that there were three stages of change: the Motivation stage, the Action stage and the Prompts stage (Dixon and Johnston, 2010). Once the three stages of change were identified, the HBCC Framework allocated the 89 health-relevant BCTs to the stage(s) they were considered most suitable for (Dixon and Johnston, 2010), see Figure 1.
Self-determination theory
Self-determination theory (Ryan & Deci, 2000) provides an underpinning to the MAP model. It seeks to understand motivation in terms of autonomy, competence, and relatedness. The theory differentiates between behaviours that are internally motivating for a person, and those from an external source (e.g., a rule or regulation). For change to be meaningful and sustained, it stresses the importance of a person’s sense of choice, their belief in their own capabilities, and a sense that the behaviour is valued by others they are connected to, even when integrating an externally-motivated behaviour into their farm routine. Bard (2018) stressed the value of integrating self-determination theory into veterinary practice and in informing interventions to change on-farm practices, given the introduction of new regulations and the shift in role of the veterinary practitioner towards preventative medicine and on-farm shared decision-making.
Fold your arms in the usual way that you fold them. Then uncross them and try to fold them with the opposite arm on top. This is an example to illustrate another theory informing the MAP model - dual processing theory. The theory states that there are two types of thinking: automatic thinking and rational, slow thinking. Making a change to behaviour (like changing how you fold your arms) takes thought, planning and problem solving – processes that happen in the Motivation and Action stages of MAP. This then takes further work, and possibly overcoming barriers, to move the behaviour into something you do automatically or on impulse – the Prompts stage of MAP.
Figure 1. The structure of the MAP model; used with written permission from NHS Education for Scotland.
What does a MAP-guided consult look like?
If a client is identified as being in the Motivation stage of change, they are exploring why they would make a change to their behaviour, and so the conversation is focused on improving their motivation. A useful BCT when a client is in the Motivation stage of change, is helping the client to explore the pros and cons of change (NES, 2022). This might be where that consult ends – you have worked with the client to explore why they might wish to make a change in the future.
In the Action stage, the client is ready to change their behaviour, but is unsure how to go about it, so the conversation is focused on helping the client to act. A useful BCT when a client is in the Action stage of change is action planning, where a detailed plan of the new behaviour is made (NES, 2022).
In the Prompts stage, the client has made attempts to change their behaviour but is finding it difficult to make it a habit or automatic, so the conversation is focused on embedding the behaviour into the client’s routine (NES, 2022). A common BCT to use in the Prompts stage is habit formation, where a new behaviour might be paired to an existing automatic behaviour, so it is easier to complete (NES, 2022). An example of this would be when to improve medication adherence, a patient places their medication beside their toothbrush – something that is already embedded in their daily routine.
For example, suppose that, in a farm setting, you have identified that wearing disposable gloves would greatly improve on-farm hygiene and reduce the spread of mastitis. After gathering information, if you feel that your client is still ‘on the fence’ about the benefits of wearing gloves and is still in the Motivation stage, you might encourage them to weigh up the pros and cons of making this change. But if you feel that they are motivated to make this change already, you might put together an action plan with your client– what gloves are going to be worn, when exactly are they going to be worn, who needs to wear them and for doing what? Finally, if the client reports that they have already tried to routinely wear gloves but they keep forgetting to put them on, you might explore with them where on the farm you could place the gloves as a visible reminder, or even engage in habit formation by pairing it to a behaviour that is already automatic, such as putting on protective clothing or hand washing.
What are the benefits of MAP model-training?
Bull and Dale (2020) delivered a blended learning-style training programme grounded in the MAP model to 177 health and social care professionals based in Northeast Scotland. The programme offered person-centred communication skills training and focused on training professionals to effectively administer five BCTs; pros and cons, information about health consequences, action planning, prompts and cues, and self-monitoring of behaviour (Bull and Dale, 2020; Michie et al., 2013). The programme was found to be highly acceptable to attendees and resulted in a significant increase in attendees’ perceived competence, self-confidence, and intention to have effective behaviour change conversations (Bull and Dale, 2020).
How useful is the MAP model?
Several studies have examined veterinary communication approaches, finding that they often consist of questioning, information gathering, and persuasion (Svensson et al., 2019; Ritter et al., 2018; Bard, 2017). While this style of communication may be useful during diagnosis and treatment-based conversations, when it comes to discussing issues which require changes to the farm routine or farm behaviours, farmers report that they favour a more collaborative approach, where their unique circumstances are explored and understood, as reflected in self-determination theory (Bard et al., 2019; Ryan & Deci, 2000). The MAP training programme provides learners with skills to:
gather information on the specific client and their farm,
support a collaborative working relationship, and,
work through ambivalence towards change through using techniques used by psychologists in practice.
It also provides a simple, practical framework to identify a person’s stage of change and tailored support based on that stage.
Research currently being conducted in the Teagasc-AHI funded AMU-FARM project is exploring the training of vets and Teagasc advisors in this approach, promoting behaviour change relating to antimicrobial use on dairy and pig farms. A first MAP of Behaviour Change training programme was delivered to a cohort of Teagasc advisors in December 2022, with further veterinary practitioner training delivered in January 2023. In addition, recent TASAH training delivered by AHI on the CellCheck and Pig HealthCheck programmes has incorporated elements of the MAP model, supporting veterinary practitioners and other professionals working in animal health to embed BCTs into their TASAH consults.
Conclusion
As the role of the veterinary practitioner is that of an advocate for change, training, research, and interventions using evidence-based behaviour change communication strategies could be beneficial. One promising strategy is the MAP model, which is a simple, evidence-based tool, which can be utilised during behaviour change client conversations of any length.

If you would like to receive information on upcoming behaviour change training delivered by Animal Health Ireland, please follow the link below or scan the QR code (left) on your phone.
1. The MAP model cannot be used during short, opportunistic consults with clients…
A. True
b. False
2. Which BCT is most useful when a person is at the Motivation stage of MAP?
A. Pros and cons
b. Action planning
C. Habit formation
3. Your client says that they would like to start vaccinating for Salmonella but are not sure where to start. What stage of MAP do you think they are in?
A. Motivation
b. Action
C. Prompts
4. Your client has introduced a foot bath to their hygiene practices but keeps forgetting to use it when entering the shed. Which BCT would help them most?
A. Pros and cons
b. Self-monitoring
C. Habit formation
5. All three stages of MAP need to be used during each consult…
A. True
b. False
Answers: 1B; 2A; 3B; 4C; 5B