Osteoarthritis in cats
About 40% of all cats have clinical signs of osteoarthritis but often these signs are infrequently recognised and, as a result, the condition is underdiagnosed. In part one of a two-part series, Sorrel Langley-Hobbs MA BVetMedDSAS(O) DipECVS FHEA MRCVS, chair in small animal orthopaedic surgery, RCVS specialist in small-animal surgery and Dr Edwina Gilldea MVB MRCVS, Zoetis companion animal veterinary lead, outline the prevalence, diagnosis and treatment of the condition
Osteoarthritis (OA) in the cat is a very common condition with 40% of all cats having clinical signs and >90% of cats older than 12 years’ showing radiographic evidence of OA.1,2 The condition is not exclusive to older cats and clinical studies have shown that even cats as young as two years’ can suffer from OA. However, as a disease, the clinical signs are infrequently recognised by pet owners and the condition is under diagnosed by the veterinary profession, with only 13% of affected cats globally being diagnosed.2 As veterinarians, we should be assessing cats for its presence and educating owners to recognise the signs (see Figure 1). Starting to screen cats as early as seven to 10 years of age will help to establish a baseline of ‘normal’ for that cat and may uncover OA early in the disease. Active screening and early identification can increase the number of impacted cats treated and improve the quality of life of cats suffering from the pain and reduced mobility associated with OA.
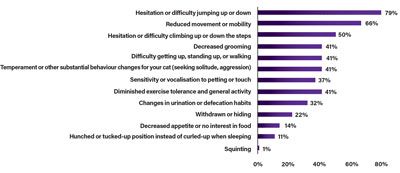
Figure1: Clinical signs associated with osteoarthritis in the cat.2
What is osteoarthritis?
Degenerative joint disease refers to damage in both the appendicular and axial skeletal systems, with most of the cases diagnosed as osteoarthritis. OA implies a joint problem, primarily associated with degeneration and loss of cartilage and proliferation of bone in the form of osteophytes around the joint. This results in a joint that has a reduced range of motion and one that is undergoing low grade inflammation resulting in varying degrees of pain and swelling of the offending joint(s). It is common in cats where multiple joints are impacted. In cats, OA usually occurs as a primary problem with no easily identifiable underlying cause, but it can also occur secondary to underlying developmental joint disease such as hip dysplasia (see Figure 2) or subsequent to a joint injury such as an intra-articular fracture or luxation. Cats develop osteoarthritis in all their large joints, but particularly the hip, hock and elbow joint3,4 (see Figure 3). Over 80% of cats older than 12 years of age had axial skeletal changes.4 Appendicular skeletal changes are even more common with over 90% of cats of all ages having radiographic changes in at least one joint.3

Figure 2. Hip osteoarthritis in an eight-year-old domestic short-haired cat secondary to hip dysplasia. Large bilateral osteophytes are present on the cranial acetabulum.

Figure 3: Elbow osteoarthritis in an 11-year-old Burmese cat. There are peri articular osteophytes and joint mice. Bilateral elbow changes were present.
Veterinarians globally report that decreased agility and reduced mobility are the most common signs reported to them for cats diagnosed with OA. Behavioural changes are also common and usually associated with the cats’ decreased agility and reluctance to move around.5,6 Cats presenting with behavioural problems can be easy to miss and is another reason to screen all cats for OA around seven to 10 years of age. These findings are in line with published studies on feline OA.
How to diagnose osteoarthritis
Owners may believe that it is normal for their older cat to sleep more and be less active or may only notice more severe signs of OA pain. As veterinarians we need to be aware of the high incidence of OA in cats and not dismiss an owner’s observation that their cat cannot jump as high anymore as being normal for an older cat. If the cat is in pain and unwilling to move around because of osteoarthritis, then it is important to educate owners as to this possibility and to try to intervene to alleviate some of the pain that the cat is experiencing. The good news is, cat owners are interested in learning more about OA in cats. In a global survey, when educated on OA as an extremely common, painful disease that could be treated, 53% of cat owners found the information relevant to their cat, and 39% were motivated to make an appointment with their veterinarian.2
Untreated pain has detrimental impact
- Musculoskeletal deterioration via reduced mobility/activity
- Cognitive and affective decline
- Impacts human-animal bond
- Untreated pain becomes harder to manage (central sensitisation)
- Untreated pain can impact a cat’s quality of life7
There are some useful questions that we can ask of an owner to identify cats with musculoskeletal problems (see Table 1). Alternatively, the cat owner can be asked to complete a validated questionnaire prior to the consultation and then regularly thereafter to assess response to treatment.8,9 Asking the pet owner to record their cat via video is also helpful to watch the cat move in their natural environment without the stress of being at the clinic. Early screening allows for a baseline to be set of what is ‘normal’ for that cat. This will help uncover any changes in behaviour or mobility as the cat ages.
Orthopaedic examination
Performing an orthopaedic examination of a cat can be tricky and often requires patience. There are ‘feline-friendly’ approaches to handling a cat that can be implemented in the practice.11,12 In a cat that is impossible to examine, this is another opportunity to ask the owner to videotape the cat in its home environment to assess their concerns more fully. Ask them to video the cat doing the things it finds difficult, eg. jumping or climbing stairs. In the more amenable cat, watching it walk around the consulting room and allowing or encouraging it to jump on and off a chair can be helpful to observe if there are any gait abnormalities. Following the visual observation, an examination of the joints is recommended. This is best carried out with an assistant holding the cat gently over its chest. The changes to look for in individual joints are swelling or enlargement, crepitus, decreased range of motion, and pain. However, bear in mind that not all joints will be painful and not all painful joints will have OA. The presence of crepitus, joint thickening and joint effusion has been shown to be predictive of the presence of radiographic degenerative joint disease.3
Untreated pain has detrimental impact
Have there been any changes in the cat’s ability or enthusiasm to:
-
Go up and/or downstairs
-
Use the cat flap/door
-
Jump onto or off the bed/sofa/your lap/work surfaces etc.Jump or climb into/onto its favourite bed
-
Play
-
Climb trees/fences, etc.
-
Use scratching posts (or other substrates)
Have any of the following been noticed?
-
A stiff or stilted gait (ie. less fluid, less ‘feline’ motion)
-
A limp
-
Vocalising or hissing in response to moving around or being stroked over joints
Have any of the following changes in your cat’s behaviour been detected?
-
Grumpy or less happy with people and other animals in the house
-
More withdrawn – interacting less with others in the house
-
Less active
-
Sleeping in different locations eg. on the floor
-
Not coming upstairs/into the house any more
-
Passing urine or faeces in abnormal locations e.g. beside the litter tray, other locations inside the house
-
Purring less
-
A reduced appetite
-
Changes in coat condition (eg. matted, scruffy) and/or grooming behaviour, eg. grooming less overall, neglecting certain areas (pain over joints or pain turning to groom certain areas), overgrooming certain areas (eg. due to pain over a joint)
Other miscellaneous questions
-
Any weight change?
-
Has the cat had any known trauma or musculoskeletal injuries in the past?
-
Any knowledge concerning affected relatives (eg. hip dysplasia is more common in certain breeds, eg. Maine Coon and possibly other pure-breed cats)?
Confirming the diagnosis
Although the combination of appropriate clinical signs and physical examination findings may lead you to be fairly certain a cat has OA, it is ideal to try to confirm your suspicions by seeing radiographic changes. The primary radiographic change associated with osteoarthritis is the presence of periarticular osteophyte formation, although this is not always present or easily identifiable in every case. It is important to appreciate that osteoarthritis may be present in the absence of obvious radiographic changes. Contrarily, the presence of radiographic changes does not always correlate with clinical signs of OA nor the degree of pain suffered. Occasionally, cats develop excessive periarticular mineralisation and ossified bodies adjacent to their joints, particularly in the stifle joint (see Figure 4).
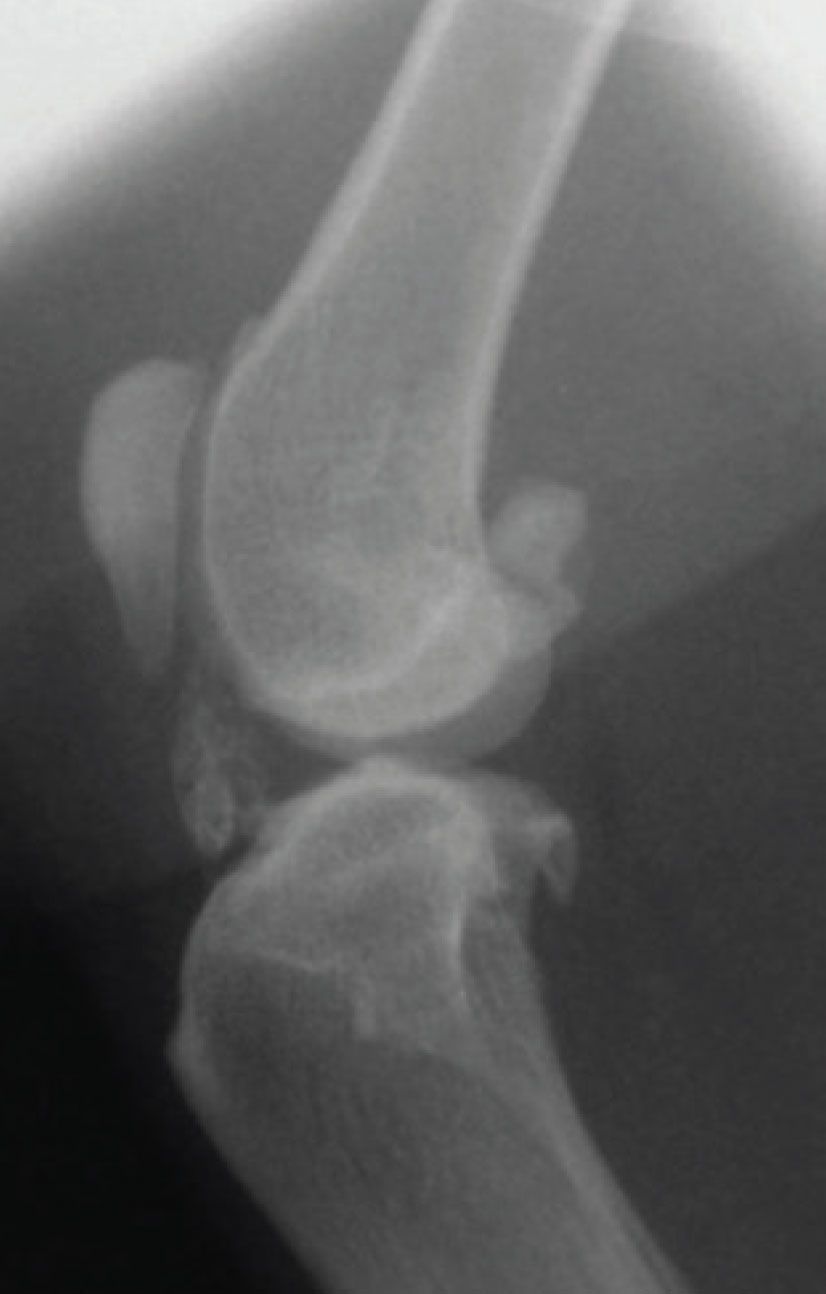
Figure 4: Mineralisation of the intra-articular structures in the stifle of a seven-year male neutered cat. There is also mild periarticular osteophytosis of the stifle with new bone on the proximal pole of the patella and trochlear ridge.
This article was adapted from a Zoetis technical bulletin: Feline Osteoarthritis, a Common and Painful Disease: Diagnosis, Treatment, New Resources and Future Options.
-
Brown D et al. What can we learn from osteoarthritis pain in companion animals? Clinical and Experimental Rheumatology. 5 (Suppl. 107):S53-S58. 2017
-
KG MarketSense 2018 Global Veterinarian Market Research
-
Lascelles BD, Dong YH, Marcellin-Little DJ, et al. Relationship of orthopedic examination, goniometric measurements, and radiographic signs of degenerative joint disease in cats. BMC Vet Res 2012;8-10
-
Hardie EM, Roe SC, Martin FR. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994-1997).J Am Vet Med Assoc 2002, 220(5):628-632.
-
Merola I, Mills DS. Behavioural signs of Pain in Cats: An Expert Consensus PLoS One. 2016
-
Bennett D, Morton C. A study of owner observed behavioural and lifestyle changes in cats with musculoskeletal disease before and after analgesic therapy; J Feline Med Surg; 2009;11:997-1004
-
Benito J et al. Owner-assessed indices of quality of life in cats and the relationship to the presence of degenerative joint disease. Journal of Feline Medicine and Surgery 14.12 (2012): 863-870.
-
Zamprogno H, Hansen BD, Bondell HD, Sumrell AT et al. Item generation and design testing of a questionnaire to assess degenerative joint disease-associated pain in cats. Am J Vet Res. 2010;71:1417-24
-
Benito J, Depuy V, Hardie E, Zamprogno H et al. Reliability and discriminatory testing of a client-based metrology instrument, feline musculoskeletal pain index (FMPI) for the evaluation of degenerative joint disease-associated pain in cats. Vet J. 2013 Jun;196: 368-73
-
Caney S. Feline Arthritis. Feline Focus, 2007, 17(3) 11-17. 11. https://catfriendlyclinic.org/vets-nurses. 12. https://catvets.com/cfp/veterinary-professionals
-
https://catvets.com/cfp/veterinary-professionals