Small animal - February 2019
Assessment of the feline blunt trauma patient
In this article, Poppy Gant BVSc MRCVS, Queen Mother Hospital for Animals, Royal Veterinary College, reviews the key steps taken in the physical examination of the feline trauma patient, highlighting common injuries and the approach to their emergency management
Cats are commonly involved in road traffic accidents. Of those that survive to presentation, some will require rapid assessment for management of life-threatening injuries. Once considered stable, it is still vital that a thorough physical examination is performed to ensure all injuries are documented.
The initial assessment of a cat involved in a road traffic accident can be separated into primary and secondary surveys. This will ensure that more dramatic injuries, such as major wounds, do not detract from abnormalities of the major body systems that are potentially life threatening. As many blunt trauma cats will have multiple injuries, a secondary survey is required to ensure all injuries are documented. This is essential for owner communications, as certain injuries may necessitate staged diagnostics and interventions, or may have implications for long-term prognosis.
PRIMARY SURVEY
The primary survey should focus on assessment and stabilisation of the cardiovascular and respiratory systems. A full neurological examination should be performed as early as possible, but this may first require basic resuscitation. During this assessment, many patients will likely benefit from active warming and supplemental oxygen therapy.
Cardiovascular
Blood loss is likely the most common cause of ‘shock’ in blunt-trauma cats. This may be challenging to detect, as cats can present tachycardic or progressively bradycardic and hypothermic. Absence of palpable metatarsal pulses, or even femoral pulses, is a useful indicator of hypotension and should prompt rapid attempts to correct hypovolaemia (Reineke 2016). Serial doppler blood pressure monitoring is useful if available, but resuscitation efforts should not be delayed while obtaining this.
All cats should be assessed for hypovolaemia secondary to haemorrhage, even in the absence of obvious external bleeding. Intracavitary bleeding, which can be assessed using point of care ultrasound, may be seen less frequently in comparison to dogs (Boysen 2004, Lisciandro 2012). A site of, often deceptively, significant haemorrhage is into the inguinal soft tissues following pelvic trauma. The author considers it rare for blunt-trauma cats to require emergency blood transfusion. However, many cats will later become anaemic if significant fluid therapy is required to correct hypovolaemia. Blood transfusions were required in approximately 20% of feline pelvic fracture patients in one referral institute (unpublished data).
If sufficient haemorrhage has occurred to cause hypovolaemia, intravenous crystalloid fluid boluses can be administered while monitoring perfusion parameters, eg. mentation, return or improvement of peripheral pulses and mucous membrane colour. One option is to administer syringes of warm compound sodium lactate (eg. 50ml for a 5kg cat = 10ml/kg) over 10 minutes. Cats are susceptible to volume overload and a full shock ‘dose’ of 40-60ml/kg is unlikely to be required. Failure to at least improve perfusion parameter after two boluses should prompt investigation for ongoing haemorrhage or other causes of shock. Where concurrent hypothermia exists, active warming should be instituted only after starting fluid resuscitation, to avoid vasodilation and worsening of hypotension.
Respiratory
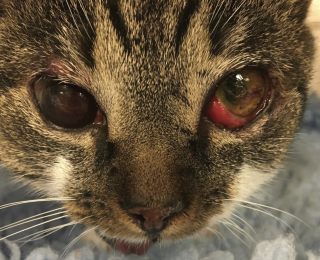
Many causes of dyspnoea are possible, and localisation is key in determining the required intervention. Thoracic trauma is common in these patients, even when there are no other visible injuries. Respiratory rate alone should not be used to exclude significant thoracic trauma and ideally survey radiographs should be performed in all patients (Figures 1 and 2) (Sigrist 2004). Table 1 gives some possible physical examination abnormalities with differentials and suggestions for diagnostics.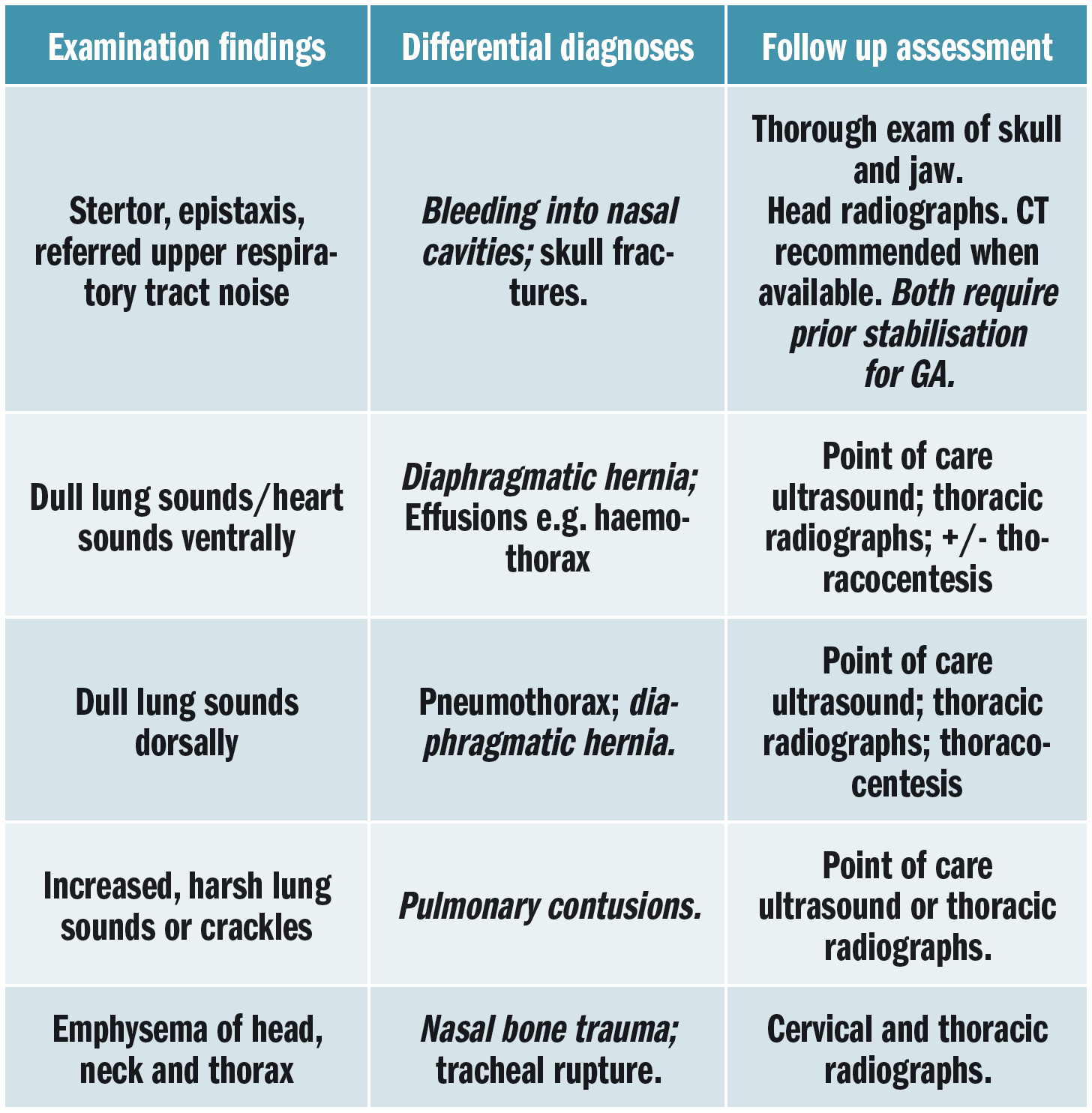
Table 1: Potential causes of dyspnoea and recommended follow-up assessment. Differential diagnoses illustrated in italics = more common.
Cats with respiratory injuries can be extremely fragile. Immediate restraint or sedation for radiographs should only be undertaken with great care. Many good resources for the use of thoracic point of care ultrasound are available (Larson 2009, Boysen and Lisciandro 2013) and can offer a much safer option for preliminary diagnostics, although potentially with reduced sensitivity when compared to dogs (Lisciandro 2012). Thoracocentesis can safely be used as both a diagnostic and therapeutic tool, particularly if a pneumothorax is suspected.
Neurological
An initial assessment of mentation and voluntary motor function (VMF) should, ideally, be performed in all cats prior to analgesia administration. However, the presence of shock may mean basic resuscitation is first required. Table 2 gives seven key areas that should be assessed in the stabilised patient, with potential abnormalities and differentials to consider.
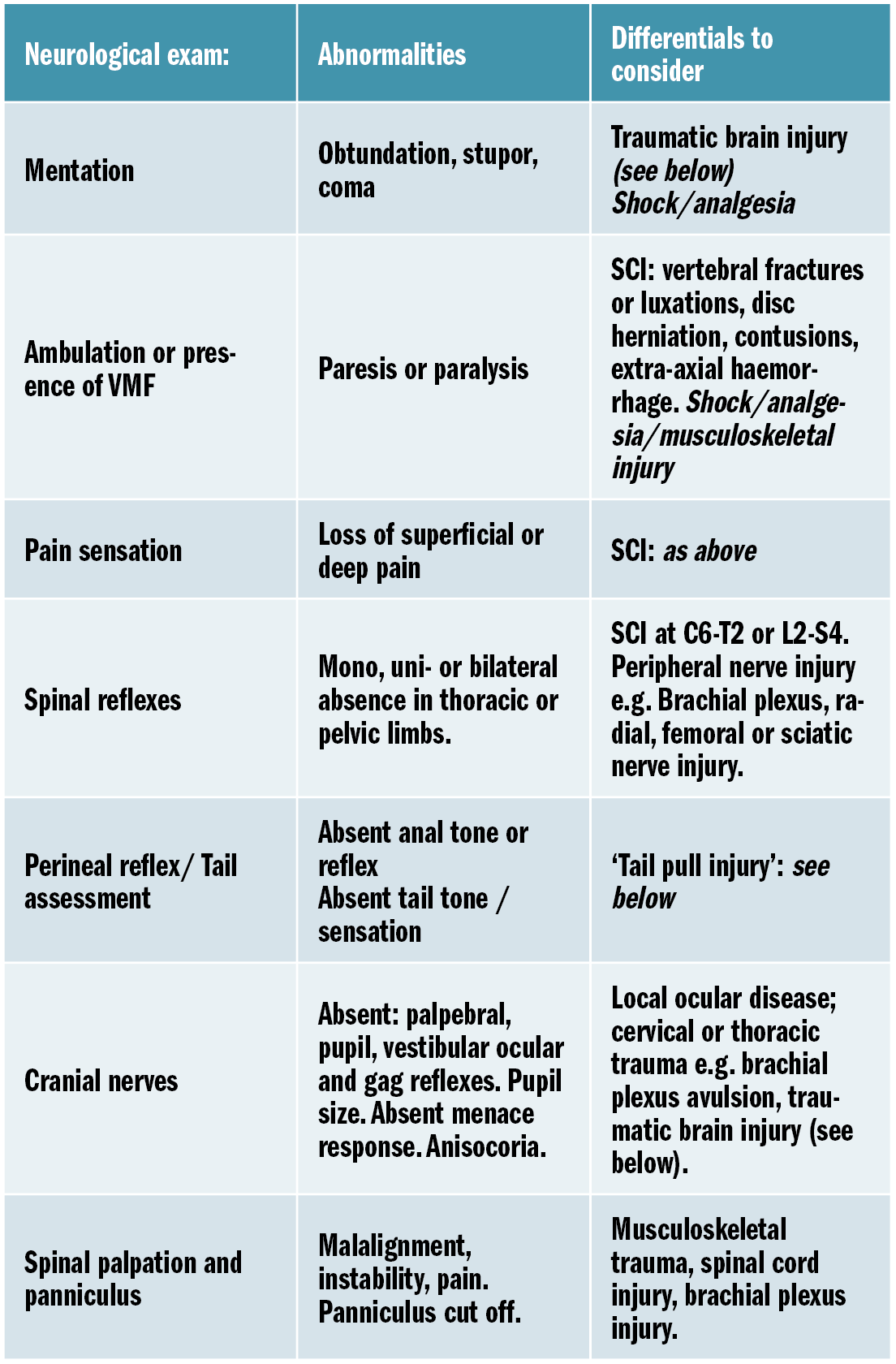
Table 2: Key abnormalities to consider on neurological exam. SCI = spinal cord injury.
Traumatic brain injury
Reduced mentation, especially in the presence of facial trauma, should prompt concern for raised intracranial pressure (ICP) secondary to brain swelling. Signs of severely raised ICP with impending herniation include bradycardia, hypertension and abnormal respiratory patterns (known as ‘Cushing’s triad’). In the conscious or mildly obtunded patient, bradycardia is more likely secondary to shock. Many resources exist discussing the management of traumatic brain injury (TBI) (DiFazio and Fletcher 2013; Garosi and Adamantos 2011) however the priorities are oxygen therapy, correcting hypotension and elevating the head. Hypertonic saline (3ml/kg) or mannitol (0.25-5g/kg – equivalent to 1.25-2.5ml/kg of a commercial 20% solution) can be considered, especially if initial crystalloid resuscitation fails to improve mentation.
Spinal cord injury
A step-wise assessment for the presence of spinal cord injury (SCI) is given below (Figure 3). If no VMF is witnessed, then significant spinal cord injury cannot be excluded. These patients should be supported on a firm surface (eg. spinal board) and movement minimised until survey radiographs can be performed to assess for unstable vertebral fractures and luxations.
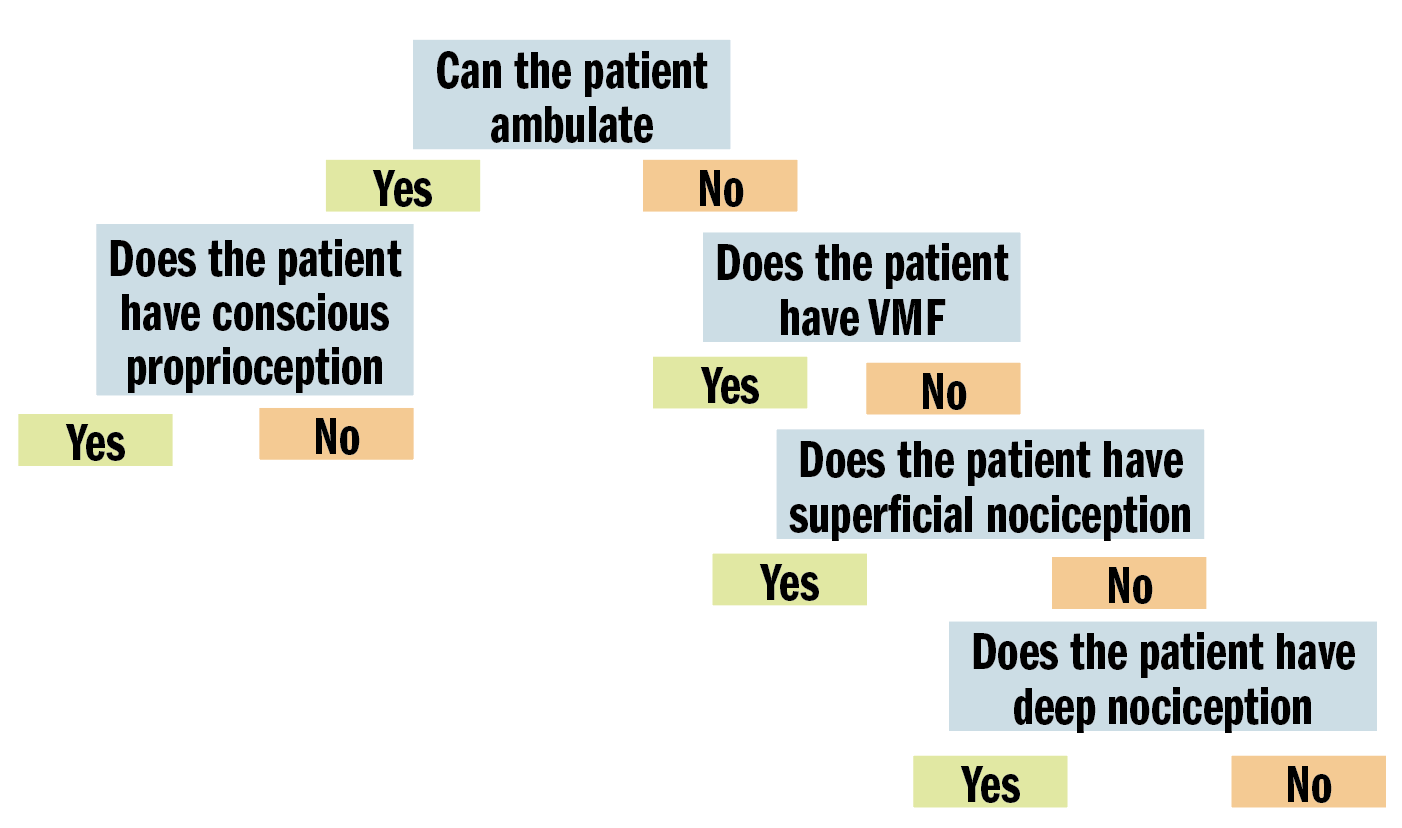
Figure 3: Step-wise assessment for presence of significant spinal cord injury.
The last step, assessment of ‘deep nociception’, can only be achieved by applying haemostats to the medial and lateral digits of the pelvic limbs. A withdrawal reflex should not be confused with a pain (cortical) response e.g. vocalisation. No data is available in cats but in dogs <5% with displaced vertebral injuries and <25% with non-displaced injuries will have functional recovery (Olby 2003). A full discussion on SCI is provided in several review articles (Eminaga et al. 2011; DiFazio and Fletcher 2013).
Tail pull injury
Luxation/subluxation or fractures of the sacrococcygeal region and stretching of the associated nerve may present as a flaccid tail with or without reduced or absent anal tone (and subsequent faecal incontinence). Absent anal tone increases the likelihood of micturition abnormalities. A lower motor neuron bladder (flaccid detrusor muscle and atonic sphincters) with continuous urinary incontinence may be seen. Alternatively, a paradoxical upper motor neuron bladder (large, difficult to express) is possible when the hypogastric nerve maintains good sphincter tone in the presence of a flaccid detrusor muscle.
Forceps should initially be applied to the distal tail to assess sensation. If no response, then forceps should be applied just caudal to the tail base. Lack of sensation here is associated with a worse prognosis for return of continence but does not preclude it (Tatton 2009). Intact perineal reflex and tail base sensation is a good indicator of early return of bladder function. Prolonged incontinence (>5 days) should prompt discussion of cystotomy tube placement to assist in longer-term bladder management, especially where concurrent pelvic fractures are present. Definitive management of fractures may be required before the outcome of continence is known. If urinary continence does not return within four to six weeks then it is unlikely to do so (Smeak and Olstead 1985). Tail function may take longer to improve and therefore early amputation is not recommended.
SECONDARY SURVEY
If no significant injuries are identified on the primary survey or the patient has been adequately stabilised, a thorough secondary survey should be performed. Common comorbidities in addition to those already discussed include those associated with the head, musculoskeletal system and pelvic injuries.
Head injury
Common injuries include jaw or skull fractures or ocular trauma. Cats with injuries to the jaw may only present with a slightly open mouth or with excess salivation (see Figures 5 and 6). Examination is normally resented and sedation or general anaesthesia may be required. Skull radiographs can be performed to investigate further but owners should be warned that only advanced imaging will allow the full extent of injuries to be determined. Examination of the jaw should include assessment of:
the mandible – both the symphysis and along the ramus;
occlusion and lateral stability of jaw related to the temporomandibular junction;
fractures of maxilla and hard palate; and dentition.
Cats with jaw fractures can be difficult to manage with a prolonged period of recovery. Other than for simple mandibular symphysis fractures, cats are often reluctant to eat and are unlikely to voluntarily meet their caloric requirements. Placement of an oesophagostomy tube should be discussed, especially if performing anaesthesia for other reasons.
Ocular injuries can range from mild globe protrusion to complete proptosis. The prognosis for vision is often not known at presentation but the presence of hyphaema is often associated with a poor prognosis (Figure 4). Globe ruptures tend to occur posteriorly and so may not be evident on physical examination (see Figures 5 and 6).
Cats can frequently present with anisocoria. This may be secondary to:
uveitis (abnormal pupil is miotic due to ciliary body spasm) – topical atropine can be applied to relieve ciliary spasm and pain (Figure 7);
Horner’s syndrome (abnormal pupil is miotic due to loss of sympathetic innervation). This is most likely second order with thoracic or cervical trauma and can often be seen with a brachial plexus avulsion (Figure 8);
optic nerve dysfunction (abnormal pupil is mydriatic due to lack of response to light); and
occulomotor nerve dysfunction (abnormal pupil is mydriatic due to loss of innervation allowing pupil constriction).
Where trauma or opioid medications mean blinking is reduced or not possible, frequent lubrication (eg. Celluvisc TM every two to four hours) should be used prophylactically to reduce the risk of corneal ulceration. Temporary procedures, for example a tarsorhaphy (Figure 6) may be required to protect the corneal surface and provide compression of retrobulbar swelling while pending any resolution of vision. A non-visual, traumatised eye should ideally be enucleated, as there is a link to primary ocular sarcomas in cats with a history of globe trauma (Zeiss et al 2003).
Musculoskeletal system
Pelvic trauma is a common finding in feline blunt-trauma patients and survey radiographs are recommended, even in ambulatory cats (Figure 9). Crepitus on manipulation of the pelvic limbs or palpation of fractures directly via rectal examination can provide an initial indication. Sacroiliac, coxofemoral and distal joint luxations, as well as long bone fractures are also fairly common and may be evident on physical examination or can be assessed on survey radiographs. The abdomen should also be carefully palpated for subtler abdominal wall ruptures (Figure 10).
Urinary system
Urinary tract rupture can also occur with pelvic injury. A palpable bladder and the ability to urinate does not exclude urinary tract trauma (Aumann 1998). Baseline blood work indicating azotaemia and hyperkalaemia and a point-of-care ultrasound indicating abnormal abdominal fluid can help confirm a uroabdomen. Abdominocentesis and fluid analysis can provide further confirmation: in one case series the mean ratio of serum to peritoneal effusion for creatinine and potassium was 2:1 and 1.9:1 respectively (Aumann 1998). The perineal area should also be assessed for subcutaneous leakage from caudal urethral ruptures, but skin necrosis may take 24-48 hours to develop. A contrast study should be performed if there is confirmation of rupture or any uncertainty of patency (Figures 11 and 12). In the author’s institute, an intravenous urethrogram is generally performed prior to a retrograde urethrogram to confirm the ureters are patent.
Wound management
Although definitive wound management may not be possible immediately, all wounds should be covered as soon as possible to minimise the risk of hospital acquired infection. Basic wound management should be performed as soon as possible, and broad-spectrum antibiotics started. It may also be appropriate to take wound culture swabs, especially with open fractures, even if these are not immediately submitted.
Analgesia and sedation/general anaesthesia for further assessment
Depending on the patient, sedation or general anaesthesia may be required to perform parts of the examination or additional diagnostics. When head trauma has occurred, these procedures should be delayed for several days if possible. In the emergency setting, sedatives that can compromise cerebral and renal perfusion, for example, medetomidine and acepromazine, should be avoided. Pure mu opioids often provide sufficient sedation, with the addition of benzodiazepines also being relatively safe. Opioids should not be withheld under any circumstances but may need to be used at lower doses.
Conclusion
Following complete assessment, all injuries and expected prognoses should be communicated to the owner. This initial discussion may be difficult given the potential requirement for multiple staged procedures with unknown prognoses. However, it is vital given the possible time and financial commitments required. Only a thorough physical examination will allow this discussion to take place and ensure owners are fully informed before committing to treatment.
Author contact
Email: pgant@rvc.ac.uk
- Aumann M, Worth L, Drobatz K. Uroperitoneum in cats: 26 cases (1986-1995). Journal of the American Animal Hospital Association.1998; 34(4):315-324.
- Barnett KC, Crispin SM. Ocular emergencies and trauma. In: Barnett KC, Crispin SM eds. Feline ophthalmology: an atlas and text. London: Saunders, 1998:17-33.
- Boysen, SR, Rozanski EA, Tidwell AS, Holm JL, Shaw SP, Rush JE. Evaluation of a focused assessment with sonography for trauma protocol to detect free abdominal fluid in dogs involved in motor vehicle accidents. Journal of the American Veterinary Medical Association. 2004; 225(8):1198-204.
- DiFazio J, Fletcher DJ. Updates in the Management of the Small Animal Patient with Neurologic Trauma. Veterinary Clinics of North America: Small Animal Practice. 2013 Jul 1;43(4):915-40.
- Eminaga S, Palus V, Cherubini GB. Acute Spinal Cord Injury in the Cat: Causes, Treatment and Prognosis. Journal of Feline Medicine and Surgery. 2011. 13(11):850-62.
- Garosi L, Adamantos S. Head Trauma in the Cat: 2. Assessment and Management of Traumatic Brain Injury. Journal of Feline Medicine and Surgery. 2011 Nov;13(11):815-23.
- Larson MM. Ultrasound of the Thorax (Noncardiac). Veterinary Clinics of North America: Small Animal Practice. 2009;39(4):733-45.
- Lisciandro GR. Evaluation of initial and serial combination focused assessment with sonography for trauma (CFAST) examination of the thorax (TFAST) and abdomen (AFAST) with the application of an abdominal fluid scoring system in 49 traumatized cats. J Vet Emerg Crit Care 2012;22(2):S11.
- Olby N, Levine J, Harris T, Munana K, Skeen T, Sharp N. Long-term functional outcome of dogs with severe injuries of the thoracolumbar spinal cord: 87 cases (1996-2001). Journal of the American Veterinary Medical Association 2003; 222: 1502-3.
- Reineke EL, Rees C, Drobatz KJ. Prediction of systolic blood pressure using peripheral pulse palpation in cats. - PubMed - NCBI. Journal of Veterinary Emergency and Critical Care. 2015 Nov 20;26(1):52-7.
- Smeak, D.D, Olmstead, M.L. Fracture/Luxations of the Sacrococcygeal Area in the Cat: A Retrospective Study of 51 Cases. Veterinary Surgery. 2nd ed. 1985 Oct;14(4):319-24.
- Schmiedt C, Tobias KM, Otto CM. Evaluation of Abdominal Fluid: Peripheral Blood Creatinine and Potassium Ratios for Diagnosis of Uroperitoneum in Dogs. Journal of Veterinary Emergency and Critical Care (San Antonio). John Wiley & Sons, Ltd (10.1111); 2001 Dec 1;11(4):275-80.
- Tatton B, Jeffery N, Holmes M. Predicting recovery of urination control in cats after sacrocaudal injury: a prospective study. - PubMed - NCBI. Journal of Small Animal Practice. 2009 Oct 8;50(11):593–6.
- Zeiss CJ, Johnson EM, Dubielzig RR. Feline intraocular tumors may arise from transformation of lens epithelium. Veterinary Pathology. 2003; 40(4):355-362.
1. Which of the following would be most likely in a blunt trauma cat with dull ventral lung sounds on auscultation?
a. Pulmonary contusions
b. Skull fractures
c. Diaphragmatic hernia
d. Pneumothorax
2. Which of the following treatment protocols would be most beneficial for a patient with suspected head trauma?
a. Hypotonic saline, oxygen therapy, head elevation, active warming
b. Hypertonic saline, oxygen therapy, head elevation and active warming
c. Mannitol infusion, manual ventilation, pelvic elevation and active warming
d. Normal saline, manual ventilation, pelvic elevation active warming
3. A blunt-trauma cat presents with a palpable, soft bladder and urine in the carrier. Which of the following differentials is most likely?
a. Bladder rupture
b. Urethral rupture
c. Tail pull injury
d. May be any of the above
4. A cat presents with anisocoria with a miotic right pupil and mid-size left pupil. Which of the following is most likely?
a. Traumatic uveitis of the right eye
b. Caudal rupture of the right globe
c. Right sided horner’s syndrome
d. Periocular trauma around the left eye
5. Which of the following is most appropriate for sedation of a blunt trauma cat to allow further diagnostics?
a. Methadone and acepromazine
b. Methadone and midazolam
c. Butorphanol and medetomidine
d. Butorphanol and midazolam
ANSWERS: C, B, D, A, B.