Steroid responsive meningitis-arteritis in dogs
Boyd Jones BVSc, FACVSc, DECVIM-Ca, Emeritus Professor in Small Animal Clinical Studies, UCD, reviews aspects of steroid responsive meningitis-arteritis in dogs
Meningoencephalitis of unknown origin embraces a number of conditions in dogs that have similar clinical signs but each has unique neuropathology. Diagnosis for the clinician can be difficult because there are no definitive diagnostic tests, thus diagnosis is based on findings from a variety of diagnostic investigations the results of which collectively support a diagnosis. The most common of them is Granulomatous Meningoencephalitis( GME) which has been reviewed previously in the Irish Veterinary Journal (O’Neill et al 2005). Steroid responsive meningitis-arteritis (SRMA) is a distinct entity in the group of meningoencephalitides of unknown origin and it is the purpose of this paper to review aspects of this condition to help clinicians make a diagnosis and treat an affected dog.
SRMA is an immune mediated inflammatory disease primarily affecting the leptomeninges and associated arteries. It is also known by other names: beagle pain syndrome, aseptic suppurative meningitis, necrotising vasculitis and others. SRMA is the established and most widely-used nomenclature which represents the clinical and pathological features of the disease. The acute form of the condition is the most common but there is a more chronic form of SRMA which is seen following relapses of the acute disease and/or after inadequate treatment. There are a number of reviews and updates about the condition which readers may wish to consult: Lowrie (2010), Tipold and Schatsberg (2010) and Rose (2019), Grapes et al. (2020), Hilpert et al. (2020) and Andersen-Randberg et al. (2021).
Who gets it?
SRMA occurs in any breed, most commonly in young dogs under two years old. Beagles, Boxers, Weimaraners, and Jack Russell Terriers are at increased odds of developing SRMA. Bernese Mountain Dogs, English Springer Spaniels and Nova Scotia Duck Tolling Retrievers are predisposed and Golden Retrievers and Wirehaired Pointing Griffons seem selectively affected in USA (Lau et al. 2019), but any breed can be affected. In New Zealand, it was young Weimaraners, six to 18 months of age, that were the predisposed breed for me.
What are the clinical signs?
The main clinical sign is profound cervical pain with guarding of the neck, a hunched posture and stiff gait. There is fever, depression and inappetence. The pain is most severe when you try to touch the chin to the chest. The history might reveal that the signs have waxed and waned or have been episodic and there has been a temporary improvement sometimes inappropriately linked to treatment e.g., antibiotics. Lumbar pain is present in some dogs. The signs of SRMA are due to meningeal inflammation but other organs can be affected including joints with polyarthritis, joint pain and effusion. In the acute form, the neurological examination is often normal except for the signs of pain. Dogs with the chronic form of SRMA have the above signs but also have additional neurological findings including paresis, ataxia, menace response deficits, anisocoria, Horner syndrome, cranial nerve VII deficits or other neurological signs.
What is the cause?
SRMA is an immune mediated disease but its aetiopathogenesis is not known. The characteristic lesion of SRMA is a fibrinoid arteritis of the leptomeninges with the predominant lesions in the spinal cord meninges rather than those of the brain. In chronic cases, there is evidence of haemorrhage, thrombosis, fibrosis, nerve root degeneration and infarction of nervous tissue which explains the more severe clinical signs (Tipold and Schatsberg 2010). Studies have looked at possible triggers including demographic, social, environmental and medical factors but breed was the only significant predisposing factor (Lowrie et al., 2009). The time of year, sex, neuter status, infectious diseases and concurrent diseases were not correlated with the risk of developing SRMA (Rose et al. 2014; Rose and Harcourt-Brown 2013). Importantly, there was no correlation between the type or timing of vaccinations and risk of developing SRMA. An aberrant immune response directed against the central nervous system is most likely with a breed predisposition. Neutrophilic pleocytosis in SRMA seems to be facilitated by chemotactic factors in cerebrospinal fluid (CSF) and upregulation of integrins and metalloproteinases that disrupt the blood brain barrier. Upregulation of IgA, induced by the Th2 immune response, also has a central role in the pathogenesis of SRMA (Tipold and Schatsberg 2010). Work by Marolini et al. (2012) implicated the expression of Toll-like receptors (TLR4 and TLR9) in enhancing the autoimmune inflammatory process and that an infectious agent can only trigger the disease. We will continue to watch this space!
How is SRMA diagnosed?
There is no disease marker for SRMA. A diagnosis is normally made on the basis of excluding other causes of spinal pain in young dogs including intervertebral disc protrusion/extrusion, syringomyelia, spinal neoplasia, cervical spondylomyelopathy, immune-mediated polyarthritis and other meningoencephalomyelitis of unknown aetiology and others (De Strobel et al. 2019; Grapes et al. 2020). With the characteristic clinical signs, laboratory findings are useful for supporting the diagnosis. There is usually a leucocytosis with left shift, hypoalbuminemia and hyperglobulinemia. Acute phase proteins including C-reactive protein (CRP) and alpha 2 macroglobulins are elevated in serum of affected dogs. This finding is not specific for SRMA but changes in serum CRP can be used to monitor treatment rather than undertake repeat CSF sampling (Biedermann et al., 2016).
Radiographs of the vertebral column are normal in SRMA cases. Where computed tomography (CT) and magnetic resonance imaging (MRI) are used in SRMA cases, images may be normal or there may be some increased contrast enhancement in the meninges. Advanced imaging, if available, is best used to rule out other conditions. If there are characteristic clinical signs of SRMA in a young dog then CSF analysis is far more rewarding for diagnosis than MRI or CT.
CSF is often grossly abnormal with cloudiness due to the increased nucleated cell count and/or protein, or is pink/yellow from acute or chronic haemorrhage. The pleocytosis is often marked – in the region of hundreds to thousands of nucleated cells per µL CSF (normal: <5 cells/µL), and CSF cytology shows a characteristic neutrophilic pleocytosis with a neutrophil percentage often over 80 per cent. The neutrophils are typically nondegenerate. No bacteria are seen in the acute disease and bacterial culture of CSF is negative. In the more chronic cases of SRMA, mononuclear cells (macrophages, lymphocytes) are also present in a mixed-cell pleocytosis.
IgA concentrations are increased in the CSF which supports the diagnosis with a high sensitivity but low specificity. This finding thus helps differentiate SRMA from other idiopathic and infectious meningoencephalitides (Tipold and Schatsberg 2010). IgM and/or IgG may also be elevated in CSF.
Finally, for some dogs where the clinical signs may be characteristic of SRMA, the CSF findings may be very mild which makes diagnosing SRMA challenging in those patients: back your clinical judgement.
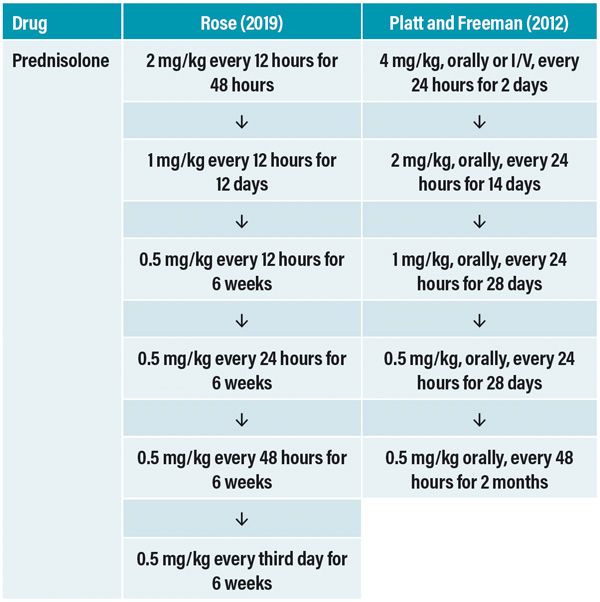
Table 1: Two plans for treatment of steroid responsive meningitis-arteritis (SRMA) with prednisolone where the move to a reduced dose of prednisolone or increased dose interval is dependent on the presence of clinical signs of improvement.
Treatments
The mainstay of treating SRMA is immunosuppressive doses of glucocorticosteroids with administration of high dose steroids IV or orally, the dose being reduced after the dog shows improvement in the first one to three days. Improvement is often dramatic, but steroids should be continued at tapering doses for a minimum of six months at least. There are no trials assessing differing treatment plans that have been statistically appraised (Rose 2019). Therefore, you have to accept the experience of veterinarians who have treated the disease. See Table 1 (overleaf) for two plans regarding steroid treatment. My preferred treatment was dexamethasone sodium phosphate administered IV at 0.5mg/kg/day, and after two to three days once there was improvement, beginning prednisone at 2mg/kg/day orally, then tapering the dose down over the next six months to alternate day administration; it worked. Revisits at intervals, every four to eight weeks are important to assess the response to treatment and whether the dog is tolerating the long-term steroid therapy. Elevated CRP concentrations may be used to reliably monitor response to therapy (Bathen-Noethen et al. 2008; Lowrie et al. 2009). SRMA is one of the few immune mediated neurological diseases that is treated with steroids alone. Some neurologists do add a second immunomodulatory agent such as azathioprine, leflunomide or cytosine arabinoside at the start of treatment (Gunther et al. 2020), while other neurologists include such agents only in cases of refractory disease or relapse. There is no evidence to support one approach over the other (Lau et al. 2019; Hilpert et al.,2020).
What is the prognosis?
Early diagnosis of SRMA is critical for successful long-term management. The prognosis is fair to good for most dogs with 80–100 per cent responding to the initial treatment using immunosuppressive steroids. While this initial response is expected, 20–30 per cent of dogs will relapse, most often following cessation of steroid treatment but some also can relapse as the steroid dose is reduced (Bierdermann et al., 2016). Dogs that relapse may respond to the reintroduction of steroid therapy alone or to a combination with another immunomodulatory drug. Once you have a response, slowly reduce the steroid dose and wean off therapy. Unfortunately, some dogs may require some form of lifelong steroid therapy, sometimes with unwanted side effects.
The prognosis is more guarded in protracted, relapsing and chronic SRMA cases where therapy requires more aggressive long-term immunosuppression (Tipold and Schatsberg 2010; Lau et al. 2019).
Acknowledgements
A version of this paper was first published in Companion Quarterly, the official newsletter of the Companion Animal Veterinarians Branch of the New Zealand Veterinary Association; Companion Quarterly 32(1), 24-26, 2021. It is republished with permission of the editor.
References available on request
1) The only significant predisposing factor for SRMA is?
A. Breed
B. Concurrent disease
C. Type or timing of vaccination
D. Neuter status
2) Which of the following breeds are not at increased risk of developing SRMA
A. Weimaraner
B. Beagle
C. Pug
D. Boxer
3) Which of the following group of clincal signs do not fit a diagnosis of SRMA?
A. Fever and inappetence
B. Cervical pain, vomiting and abdominal pain
C. Cervical pain, hunched posture, stiff gait
D. Waxing and waning/episodic signs
4) The most useful diagnostic test to confirm a diagnosis of SRMA in a young dog is?
A. Magnetic resonance imaging
B. Serum C reactive protein concentration
C. Serum IgA concentration
D. CSF cytology and analysis
5) The mainstay of treating SRMA is administering?
A Azathioprine
B. Cytosine arabinoside
C. Immunosuppressive doses of glucocorticoids
D. Low dose glucocorticoids
Answers: 1A; 2C; 3B; 4D; 5C.